Managing Prolapse During Pregnancy
posted on February 18, 2022
What is THAT?! I thought to myself as I squatted over a mirror at 8 weeks postpartum, shocked by what I was seeing “down there.”
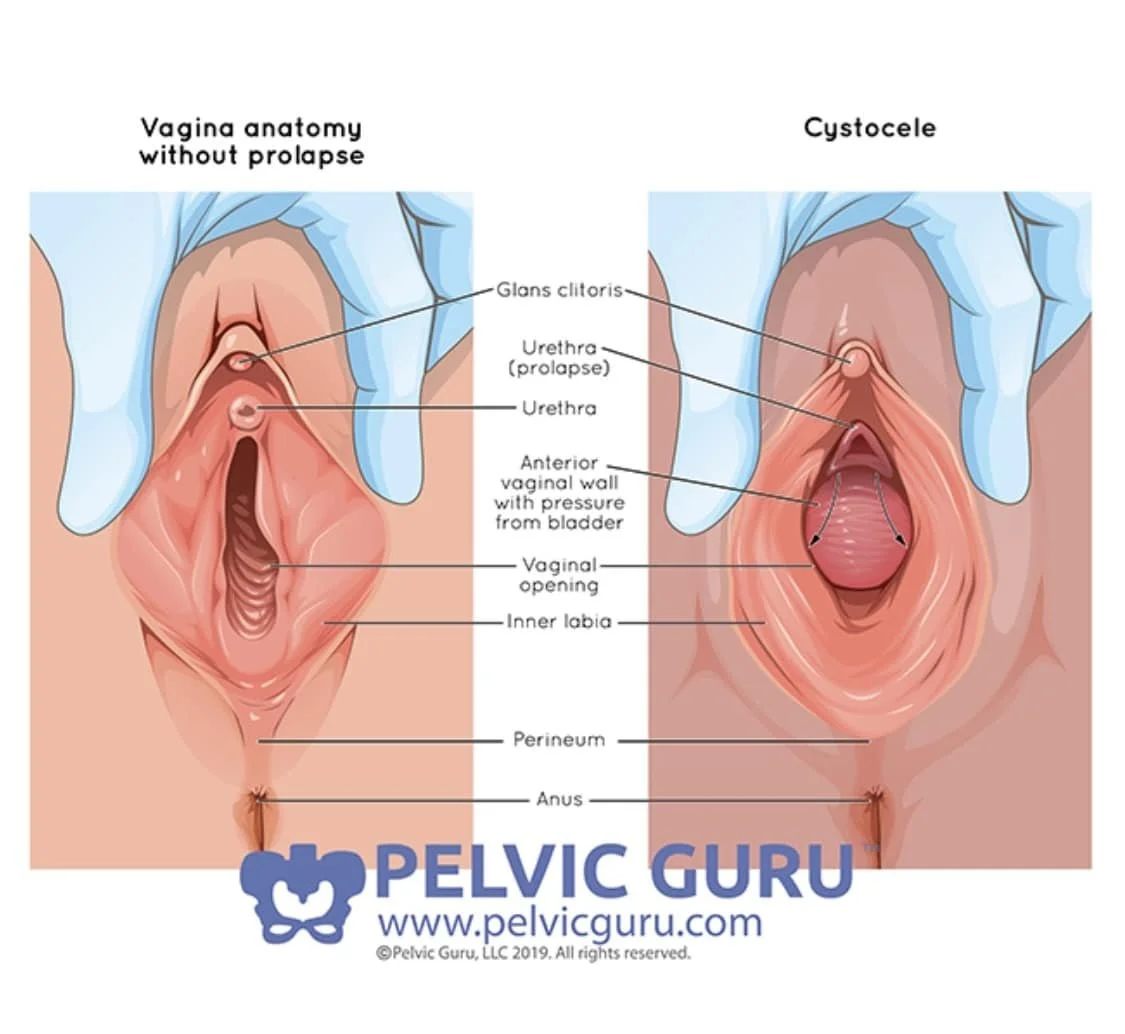
I had Pelvic Organ Prolapse (POP). Cystocele, or prolapse of the bladder, to be exact. And I shouldn’t have been shocked. I had been been experiencing heaviness and bladder urgency for weeks.
My Personal Experience with Prolapse
I felt like my vagina was falling out. However, at my 6 week postpartum visit, my OB made no mention of prolapse to me, even when I brought up my symptoms to her. Besides having granulation tissue that needed to be treated, everything “looked good.” I got the all clear and was sent home and told to call if I had any issues.
Two weeks later, I discovered my prolapse and immediately panicked. I thought, “Oh maybe this is just more of that granulation tissue that needs to be treated.” But then I quickly realized, “No, Nicole. This is the inside of your vagina making its way to the outside of your body.”
In case you were wondering, here’s a little visual of what I saw….
Image from pelvicguru.com
Luckily for me, my prolapse wasn’t fully hanging down outside of my vagina. I had what they call a Stage 2 Cystocele, where the anterior vagina wall descends to the opening of the vagina due to pressure from the bladder. My symptoms were exacerbated with standing and moving around for prolonged periods. And with bearing down, my prolapse progressed from a Stage 2 to a Stage 3, where the anterior wall starts to protrude outside.
After coming to terms with my situation, I scheduled an appointment with a Pelvic Floor Therapist and started home visits right away. I learned so much from her, but it honestly took a long time for me to heal.
Healing from Prolapse Takes Times
During vaginal delivery of my son, I experienced three 2nd degree vaginal tears, two which were internal and deep into my vaginal muscles. I learned through this experience that just because 2nd degree tears are common, it DOES NOT mean they are created equal, and they definitely should not be dismissed.
I also learned that I was more susceptible to prolapse because I have hypermobility in my joints. And with extended breastfeeding, hormones can increase tissue laxity, making healing from prolapse even more challenging. It took me a long time to heal, strengthen my core, and reconnect with my pelvic floor muscles. I had to learn how to manage pressure and make lifestyle modifications to alleviate my symptoms. Eventually, things got better and I was finally asymptomatic from POP. Hooray! I’ve learned that asymptomatic is OK when it comes to prolapse. If you bear down and still have a Stage 1-2 prolapse, but are asymptomatic when walking and moving around, that is perfectly normal and an acceptable level of healing. For many women, that is the goal and it certainly was for me!
My postpartum healing journey and experience with prolapse highly motivated me to pursue continuing education in Pelvic Floor Therapy. As an occupational therapist, I never considered this career move until I experienced these issues firsthand. I started taking courses with Herman & Wallace to treat pelvic floor dysfunction and am currently finishing up my Pregnancy and Postpartum Corrective Exercise Specialist (PCES) certification.
Fast forward to now: I’m pregnant with my second! And one of my biggest concerns going into this pregnancy was how I would manage prolapse. Around 15 weeks, I saw my Pelvic Floor PT and together we discussed strategies to manage prolapse and keep me asymptomatic throughout my pregnancy.
I’m now 21 weeks and feel very confident in those strategies and my own knowledge as Pelvic Floor OT to manage prolapse throughout the rest of pregnancy. I’m here to share those with you today.
Strategies to Manage Prolapse During Pregnancy
Pressure Management
This is probably the most important takeaway from this list. If you can’t manage pressure, you can’t manage prolapse.
So how do you do this during pregnancy?
Regular core engagement – learning how to engage your transverse abdominis muscles (TAs) is a game changer, especially during pregnancy. These are your deep core muscles, those that wrap around the lower abdomen like a corset. Coordinate engaging the TAs with your exhale breath and draw baby in towards your spine. Hold for a few seconds and then release. I have a video demonstrating this on my instagram @nicolepelvicot.
Diaphragmatic breathing – breathing not just into your chest or belly, but into your ribcage. Expand the ribcage WIDE and fill your abdomen with air like a canister. This will allow full activation of the diaphragm, which co-coordinates with the pelvic floor.
Functional pelvic floor exercises – this means not just sitting on the sofa and kegeling in a slouched posture. This means engaging your pelvic floor with functional tasks, breathing, and during exercise, like squats, lunges, and tall kneeling positions. Your pelvic floor does not work alone – it works with your entire kinetic chain, so engaging it with other muscles + breathing is best and WAY more functional. As an OT, this is very important to me 😉
Minimize bearing down – By learning how to coordinate pelvic floor contractions with your breath, you can avoid bearing down during strenuous activities or exercise. This is SO important in managing prolapse! Use your exhale breath, engage your pelvic floor and TAs, then perform the activity. This will not only help manage prolapse, but protect your back from common pregnancy aches & pains.
Lifestyle Modifications
Avoid “just because” trips to the bathroom
Avoid sitting on the toilet too long, which causes unnecessary pressure on the pelvic floor.
Avoid bladder irritants – things like caffeine, citrus foods, artificial sweeteners, chocolate, carbonated beverages, and spicy foods can all contribute to bladder urgency and irritation. For example, when I consume too much caffeine, I almost always have increased prolapse symptoms – heaviness, pressure, and urgency. I know if I want to avoid this, I need to limit my caffeine intake.
Drink lots of fluids and eat a well-balanced diet – It’s always important to drink water, especially during pregnancy, but a key benefit is staying hydrated to avoid constipation. I also take a Magnesium supplement every night to promote rest and regular bowel movements 🙂 *always consult with your provider before taking any supplements!
Mindful Movement
Regular exercise to strengthen your core, glutes, hip, and pelvic muscles is so important with managing prolapse! Throughout this pregnancy, well let’s be honest once I felt good enough to do so after the first trimester, I started mindfully moving my body with resistance training and a regular prenatal yoga practice. I switch it up throughout the week, but all of the moves are pregnancy safe and focus on core, glute, and hip strengthening. I focus on not only engaging the pelvic floor, but lengthening and relaxing it as well.
Key Takeaways
Pregnancy does not automatically mean your prolapse will get worse! I repeat – just because you’re pregnant, your prolapse does not have to get worse. You can remain asymptomatic, it just might take some adjusting! And for many, prolapse symptoms can often improve during pregnancy due to the uterus moving up.
If you do feel like you are having more symptoms as your pregnancy progresses, you have options! Reach out to a Pelvic Floor PT/OT to discuss a treatment plan that is right for you.
Lifestyle modifications are just as important as mindful movement and exercise. A few tweaks can make all the difference!
If you have experience with prolapse, how have you managed your symptoms? Did you notice a difference during pregnancy?
I hope you found this post helpful! Check out my instagram for more pelvic health tips 🙂
Talk Soon!
Nicole